“My baby isn’t gaining enough weight.”
Many of my consults start this way. But even with the same starting point, these visits can go in so many different directions, because so many factors are involved. Physical issues can come from the mother’s side or the baby’s, and there are always personal and family dynamics to consider. It’s never just about milk.
Always, much of my time is in conversation with the parents. First, is the weight gain really too low, or is this a healthy baby who happens to be on the slow end of normal? Are the right growth charts being used? Many pediatricians’ offices are still using older growth charts, which were not based on breastfed babies. And any charts are just averages. Outside of Lake Wobegone, we can’t all be above average.
I need to know also whether the baby is at the breast often enough and long enough. If you aren’t in the restaurant, you don’t get a meal. Rigid schedules from books are one problem, but aren’t the only concern – one mother described to me how she tried every possible comforting technique when her baby cried, and only if she was still crying did she feed her. Of course sometimes the baby would run out of energy before this point, so she would give up and go to sleep, missing a feeding she needed. The mom was very health conscious, and conscientious, and had no idea she was underfeeding her baby. She came from a family where overeating, and associated health problems, were common. As a child, she felt she had been encouraged to eat for comfort, and eat past the point of satisfaction, and wanted to make sure she didn’t feed her daughter unless she was truly hungry. She was reassured when we discussed how feeding on cue would actually help her daughter learn to feel full and regulate her own eating. “When in doubt, whip it out!” was my advice. It was well received, but wouldn’t have found it’s mark if we hadn’t had the whole conversation.
Sometimes there’s a medical issue that needs attention, and it can be with either mother or baby, or both. Often the mother who calls me is already assuming the problem is on her end, saying “My milk supply is low.” Which it may well be, but lactation works by supply and demand. So a baby who doesn’t drain the breast leads to a mom producing less milk. If nobody’s ordering, the chef stops cooking.
I check inside the baby’s mouth, feel his sucking pattern, and watch the way he moves his head. A tongue tie – when the tongue can’t move normally because of the way it’s attached to the floor of the mouth – may be preventing the baby from nursing efficiently. Sometimes a difficult birth or awkward position in utero has left the baby with tension in the neck and jaw that makes breastfeeding difficult. Some babies, often those born a little early, have a weak or uncoordinated suck. I may wind up referring a baby to a specialist, and teaching the parents some suck-training exercises, and feeding techniques to help compensate.
Occasionally the mother’s medical history or breast exam gives me a clue that something is off in the “kitchen.” In these cases, I’m especially glad she is pursuing help. Low milk production can be a sign of a medical condition, like low thyroid; if she just stopped breastfeeding and left it at that, a chronic problem might go undetected for years, putting her at a greater risk for long term health issues. In those cases, I’ll be referring to a physician to treat the medical issue, while working with the mother on rebuilding her milk supply, and a feeding plan to help the baby get enough nutrition meanwhile. There are a lot of ways to approach supplementing, and it’s more important that the plan be sustainable than that it be perfect.
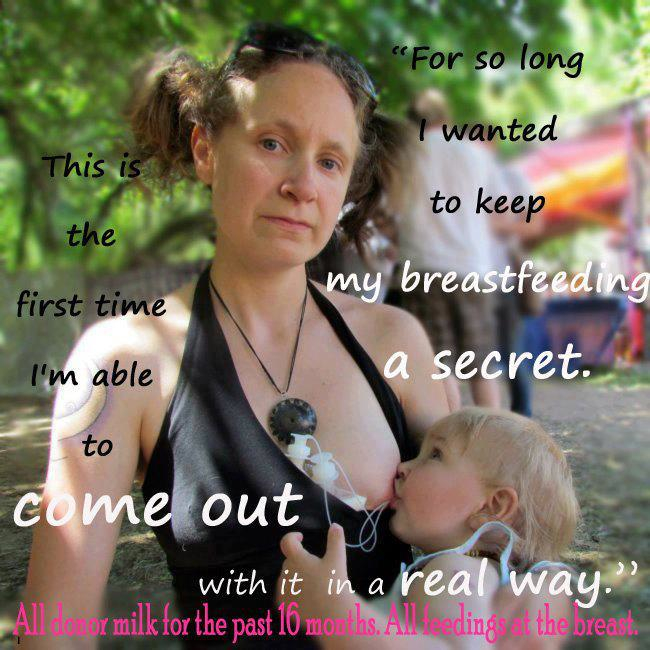
With a few mothers, I’ll have to bring up a tough subject: insufficient glandular tissue (IGT). This is when the mammary tissue did not develop fully, and can’t make enough milk as a result. This is hard news to give. The mother is likely to feel terribly disappointed, but she may also be relieved to have an answer. What I want to focus on with her is that she still has options. She might decide to give supplemental feedings at the breast. She might be interested in using donated human milk for supplemental feedings. Her milk supply may never be full, but there are ways to increase it if she wants to try. Some women are eager to maximize their milk production, others don’t want to make a project out of it. I’ll always remind her that she isn’t a milk dispenser, she’s a mother, and mention the saying “Love is not measured in ounces.” Her breastfeeding experience will be different from what she expected, but it can be rewarding, and it will be all hers.
With a few mothers, I’ll have to bring up a tough subject: insufficient glandular tissue (IGT). This is when the mammary tissue did not develop fully, and can’t make enough milk as a result. This is hard news to give. The mother is likely to feel terribly disappointed, but she may also be relieved to have an answer. What I want to focus on with her is that she still has options. She might decide to give supplemental feedings at the breast. She might be interested in using donated human milk for supplemental feedings. Her milk supply may never be full, but there are ways to increase it if she wants to try. Some women are eager to maximize their milk production, others don’t want to make a project out of it. I’ll always remind her that she isn’t a milk dispenser, she’s a mother, and mention the saying “Love is not measured in ounces.” Her breastfeeding experience will be different from what she expected, but it can be rewarding, and it will be all hers.
Not long ago, mothers with slow-gaining babies would probably have switched to formula feeding immediately, end of story. Now, more often they want to figure this out. I’m glad of that, and not only for the sake of mother and baby’s health. I hear the sadness in the stories older women tell me at parties all the time: “I really wanted to breastfeed, but my milk wasn’t enough.” They were never offered the chance to get a real evaluation, which could have solved the problem, or at least offered an explanation for why breastfeeding didn’t work. However the lactation turns out, I want my client to eventually look back on her breastfeeding experience with pride in herself – not because she did or did not lactate, but because she faced a difficult situation early in mothering, took charge, persisted, adapted, and ultimately fed her baby in whatever way she decided was best.
I love my work, because it’s not just about milk.
If you are in need of a lactation counselor or consultant, you can visit the Web sites of the Academy of Lactation Policy and Practice or the International Lactation Consultant Association. Thank you to Courtney Jarecki for permission to publish her photograph on this blog.
awesome article! This is really a super Blog!
ReplyDeleteI would like, based on my personal experience, to add three suggestions to every lactation consultants and doula's repertoire, when a mother doesn't produce enough milk:
ReplyDelete1) Ask the mother to inquire in her extended female family, whether any other members had trouble producing milk, and
2) Give the mother a timeline. Put together a repertoire of things to do, but give specific instructions. For instance: If two weeks of all of this stuff doesn't work, be ready to let go.
3) PLEASE PLEASE PLEASE let women know that it is NOT always just supply and demand. That sometimes it doesn't work no matter WHAT you do!
Here's my story - I hope it will help others... I was not producing milk. Already in the hospital, something felt wrong. Everyone told me I am crazy, and that all is fine, and I should just keep trying. I knew something was off, but I assumed they were right and I was wrong. 6 days later, still no milk coming in. In that time, I was pumping with a hospital grade pump, 3 hours a day, and producing about 5ml a day on a good day. Yes, you read this correctly.
This is when the trips to the lactation consultants began. Two different independent groups. Within a day I was on 4 different supplements, in addition to domperidone. I started using the SNS at every feeding. I pumped 4-5 hours in a 24 hours period, in addition to the SNS. Same hospital grade pump. I felt ashamed and like a failure, and everyone tried to figure out what I am doing wrong, because this *never* happens.
I did not meet the profile for IGT, and it just didn't make sense.
Finally, it was my *pediatrician* who knocked sense into me. 2.5 weeks of this, and she told me that my baby needs me more than the pump needs me, and that my baby needs me more than she needs breastmilk. She told me to set a deadline. Sobbing, I called both my lactation consultants. One told me that yeah, if in 10 days there is no improvement, it probably won't work. The other wanted 3 weeks. In the meantime, I was going crazy, was completely sleep deprived, and barely got to enjoy my new baby because I spent all her waking time pumping (right after a feeding, as instructed).
At the 2 weeks mark after starting all the treatments, I stopped. I switched to formula, and began getting to know my daughter. I still felt like a failure.
And then, at new moms groups, among the 25 women in the groups I attended, 3 couldn't produce milk (in addition to me), and one had a mother and two sisters who didn't have milk, while she herself was flowing. I asked around. Turns out my maternal grandmother never had milk.
Wow, and here I was thinking I am completely abnormal and a one in a million failure, and instead, I am hearing about failures to produce milk everywhere I go!! And these are not just "not enough milk", these are "no milk" people like me, who tried everything.
I don't know what the real stats are. I do know that:
1) I did not meet the profile for IGT
2) I tried *everything*
3) I sensed something was wrong, and got NO validation
4) There is genetic precedent in my family
5) I was checked and didn't have *any* other medical issues
6) My breasts did grow *a bit* during pregnancy, and my areola did get much darker
7) I missed, and will never get back, the first three weeks of my daughter's life, because I was a slave of the pump.
I also know that lactation issues are common enough to have been mentioned even in the bible! Wet nurses were common, and even Sarah, Abraham's wife, did not produce milk. This is not a new problem, it is real, it should be acknowledged, mothers should be warned about it, and helped through it instead of pushed into trying harder in vain.
At the end of the day, there are some benefits for breastmilk, but they are far more minor than commonly believed, and probably not worth missing your baby's first weeks for.
Good luck to all the mothers out there, and lactation consultants everywhere, please please remember my story as you meet new mothers who do not produce milk.
Thank you very much for sharing your story here. The study of lactation is a rapidly growing science -- we know much more about the causes of low milk supply than we did a generation ago (or in biblical times), and there is still more to be discovered about the underlying medical causes of this problem for mothers who have not received a clear diagnosis. This blog entry was not intended to be an exhaustive catalog of disorders which may result in low milk supply; e.g., conditions such as PCOS (Polycystic Ovary Syndrome) and other known causes of low supply were not all included in the post.
DeleteAs a Certified Lactation Counselor for the past 11 years, I cannot endorse comments recently appearing in the media which suggest that the benefits of breastmilk are far more minor than commonly believed. Breastmilk is lifesaving for babies in poor, developing countries as well as in wealthy, developed countries, and has been confirmed as a preventive measure against conditions ranging from life-threatening episodes of diarrhea to Sudden Infant Death Syndrome.
However, I do agree that as our society makes the difficult transition from being a formula-feeding society back to being a breastfeeding society, many mothers have not received the support, information, or medical evaluations they need in order to breasfeed with ease, to have access to other options like donor human milk, or make a decision to stop breastfeeding with full support for their circumstances.
As Jessica Lang Kosa points out in her guest blog post here, validation of the breastfeeding woman's reality is much more important than heaping prescriptions and judgments on her without regard to the profound emotional vulnerability of new motherhood. I, too, share your wish that we will arrive at a time very soon where no mother has to go judged and unsupported if she experiences low milk supply.
I certainly don't want to downplay your struggle. A friend had a similar experience with her first child and ended up giving him donor milk when available and supplementing with formula when necessary. She, too, was very upset about it and now with her second has been proactive to get donor milk so that her baby has had nothing but breastmilk for it's first several months. She knows that babies' bodies are born designed for and expecting breastmilk and that formula is a very inferior substitute. Of course this means that we need to do more to support women who are not able to provide their own breastmilk if they would like to make sure their babies receive breastmilk for a period of time. Both my babies had formula at various points in their babyhood so there's no judgement here for using it. Just clarification that the reality is that it is not what a baby's immune system, gut, brain, and whole body are designed to receive and is therefore going to be detrimental to some extent to their development. Fortunately humans are quite resilient (unlike calves who will almost certainly die if they do not receive their mother's colostrum) and can and do survive and even thrive with an alternative food.
DeleteAlso while it might be beneficial to ask if others in the family had problems making milk, my concern is that many women believe they didn't make enough milk because of misunderstandings or misconceptions about how to feed at the breast. I would venture to guess that far more women believe they didn't make enough milk than actually had true IGT or other physical supply issues. If a woman receives confirmation that the women in her family just don't make milk then she may not seek the help needed or even really try and her chances of feeding her baby as natured intended are sabotaged. I know a woman who was planning a VBAC. The women in her family said they (she) couldn't give birth vaginally because they'd all had cesareans. But she did have her VBAC. Then they said she shouldn't try breastfeeding because none of them made milk. But she did with no issue. What if she'd believed them though and hadn't tried to have a VBAC or breastfeed?
Also I'm a little confused about your information about Sarah. The Bible says, "Sarah said, 'God has brought me laughter, and everyone who hears about this will laugh with me.” 7 And she added, “Who would have said to Abraham that Sarah would nurse children? Yet I have borne him a son in his old age.' 8 The child grew and was weaned, and on the day Isaac was weaned Abraham held a great feast." There's no indication that she did not nurse him. In fact the Jewish Torah says that SHE had abundant milk and wet-nursed the babies of the noblewomen whose milk was dried up.
Beautiful post. As a fellow IBCLC, I work with many low supply cases. It is a physical and emotional roller coaster for many families and is always a joy and privilege to support them on their journey.
ReplyDeleteAs always, you inspire me!!!
ReplyDelete